Understanding Quest Diagnostics Billing: A Comprehensive Guide
When it comes to medical testing and diagnostics, understanding the billing process is crucial for patients and healthcare providers alike. Quest Diagnostics billing can often be confusing, especially for those unfamiliar with the nuances of insurance claims and medical payments. This article aims to demystify the billing process associated with Quest Diagnostics, providing you with the knowledge needed to navigate your medical bills effectively.
In this guide, we will delve into the various aspects of Quest Diagnostics billing, including how to interpret your bills, what to do if you encounter discrepancies, and tips for managing costs. By the end of this article, you will have a clearer understanding of the billing practices of Quest Diagnostics and how to ensure that you are being charged accurately.
Whether you are a patient preparing for a lab test or a healthcare professional seeking insights into billing practices, this article will serve as a valuable resource. We will cover essential information, including insurance coverage, patient responsibilities, and frequently asked questions about Quest Diagnostics billing.
Table of Contents
- 1. An Overview of Quest Diagnostics
- 2. Understanding Quest Diagnostics Billing
- 3. How to Read Your Quest Diagnostics Bill
- 4. Insurance and Quest Diagnostics Billing
- 5. Common Billing Issues and Resolutions
- 6. Ways to Manage Your Quest Diagnostics Costs
- 7. Resources for Further Assistance
- 8. Conclusion
1. An Overview of Quest Diagnostics
Quest Diagnostics is a leading provider of diagnostic testing services, offering a wide range of laboratory tests that are essential for patient care. With a vast network of patient service centers, Quest Diagnostics is designed to meet the needs of both patients and healthcare providers.
Founded in 1967, Quest Diagnostics has grown significantly and now operates more than 2,200 patient service centers across the United States. The company is known for its commitment to quality and innovation in laboratory testing, providing accurate and timely results that healthcare professionals rely on for patient diagnosis and treatment.
As a patient, it is essential to understand how the billing process works within this organization, as it can significantly impact your overall healthcare experience.
2. Understanding Quest Diagnostics Billing
Quest Diagnostics billing encompasses the charges for laboratory tests and services provided to patients. These bills may include various charges, such as the cost of the tests performed, any associated fees, and potential insurance adjustments.
Patients receive bills after their tests have been conducted, and the charges may vary based on several factors, including the type of tests performed and the patient's insurance coverage. Understanding these components is crucial to managing your healthcare expenses effectively.
2.1. Key Components of a Quest Diagnostics Bill
- Test Charges: The base cost of the laboratory tests conducted.
- Additional Fees: Charges for services such as specimen handling or processing.
- Insurance Adjustments: Any discounts or adjustments made based on your insurance coverage.
- Patient Responsibility: The amount you owe after insurance payments have been applied.
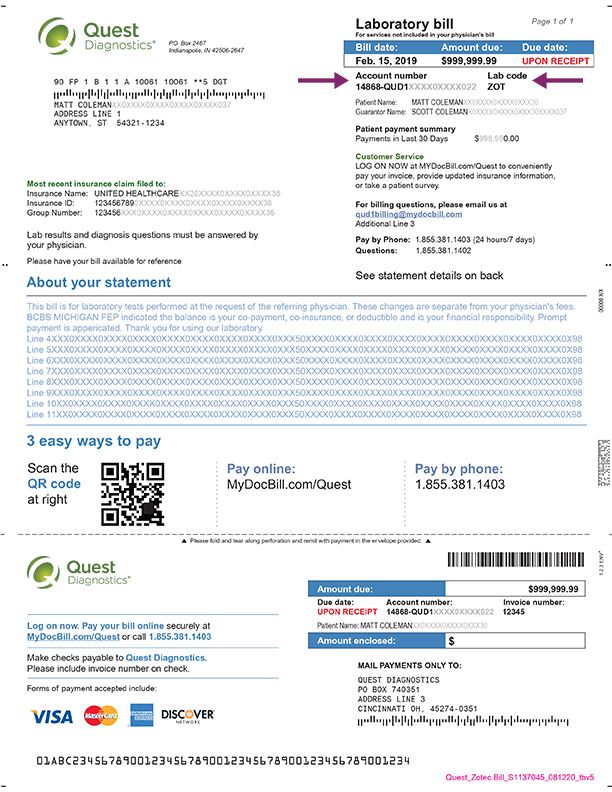
3. How to Read Your Quest Diagnostics Bill
Reading a Quest Diagnostics bill can be challenging, especially for those unfamiliar with medical billing terminology. Below are key components typically found on a Quest Diagnostics bill:
- Patient Information: Your name, address, and date of birth.
- Billing Account Number: A unique identifier for your billing record.
- Service Date: The date your tests were performed.
- Itemized Charges: A detailed list of tests conducted and their respective costs.
- Insurance Payments: The amount covered by your insurance provider.
- Total Amount Due: The final balance you are responsible for paying.
4. Insurance and Quest Diagnostics Billing
Insurance plays a significant role in how Quest Diagnostics bills its patients. Understanding how your insurance works with Quest Diagnostics can help you minimize out-of-pocket expenses.
4.1. Types of Insurance Accepted
Quest Diagnostics accepts a variety of insurance plans, including:
- Medicare
- Medicaid
- Private Health Insurance
- Employer-Sponsored Plans
4.2. Verifying Insurance Coverage
Before undergoing testing, it is advisable to verify your insurance coverage with Quest Diagnostics. This can help you understand what tests are covered and any potential out-of-pocket costs you may incur.
5. Common Billing Issues and Resolutions
Despite best efforts, billing issues can arise with Quest Diagnostics. Here are some common problems and how to resolve them:
- Discrepancies in Charges: If you notice charges that seem incorrect, contact Quest Diagnostics customer service for clarification.
- Insurance Denials: If your insurance denies a claim, review the reason for denial and consider appealing the decision.
- Payment Plans: If you are unable to pay your bill in full, inquire about setting up a payment plan.
6. Ways to Manage Your Quest Diagnostics Costs
Managing costs associated with Quest Diagnostics requires proactive steps. Here are some tips to help you:
- Understand Your Insurance Policy: Familiarize yourself with your coverage to anticipate potential expenses.
- Ask for Cost Estimates: Request estimates for tests before they are conducted.
- Utilize Preventive Services: Take advantage of preventive services that may be covered at no cost.
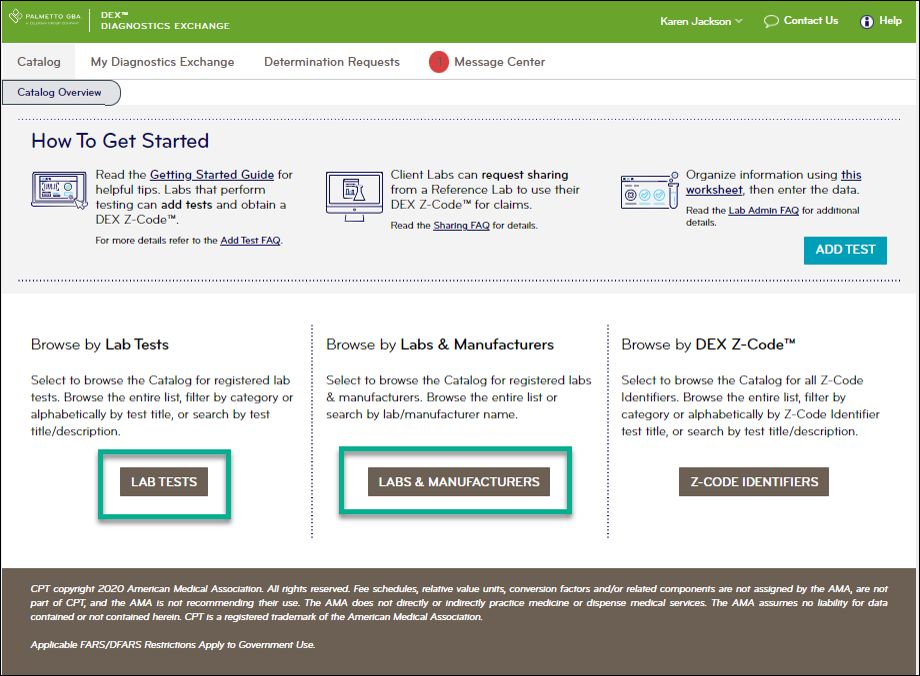
7. Resources for Further Assistance
If you require additional help with Quest Diagnostics billing, consider the following resources:
- Quest Diagnostics Customer Service: Reach out to their customer service team for billing inquiries.
- Your Insurance Provider: Contact your insurance company for questions regarding coverage.
- Financial Assistance Programs: Explore available financial assistance programs through Quest Diagnostics.
8. Conclusion
Understanding Quest Diagnostics billing is essential for effectively managing your healthcare costs. By familiarizing yourself with the billing process, reading your bills carefully, and knowing your insurance coverage, you can take control of your medical expenses.
We encourage you to share your thoughts or experiences regarding Quest Diagnostics billing in the comments section below. If you found this article helpful, consider sharing it with others or exploring more articles on our site.
Thank you for reading, and we look forward to providing you with more informative content in the future!
You Also Like
How To Make An Image Bigger Without Losing QualityWhen Should I Put Up Christmas Decorations? A Comprehensive Guide
Understanding Hive Query Language: A Comprehensive Guide
How To Make A Beautiful Paper Flower Bouquet: A Step-by-Step Guide
Exploring The Enigmatic World Of Photos Shiv: A Comprehensive Guide